EEOC Proposed Rules on Wellness Incentives
The Equal Employment Opportunity Commission (EEOC) recently proposed rules that would clarify how employers whose wellness programs have features like biomedical screenings or health risk assessments can avoid running afoul of the Americans with Disabilities Act (ADA). This is a welcome development following the controversial enforcement actions the EEOC took last year against employer wellness programs. But, some important differences remain between the Health Insurance Portability and Accountability Act (HIPAA) and proposed ADA rules that could reduce employers’ flexibility in designing wellness programs.
Under HIPAA rules, the maximum wellness reward for health-contingent programs that don’t target smoking cessation is 30% of the health plan’s coverage costs for the specific tier (self-only, self plus one, family, etc.) an employee has selected. No limit applies to participation-based wellness rewards — even if the program involves health risk assessments or biomedical screenings, as long as the incentive is awarded regardless of assessment/screening results.
However, the EEOC rules would limit the maximum incentive to 30% of the total cost (employer and employee contributions) of employee-only coverage for wellness programs that involve taking health risk assessments and/or biomedical screenings. In addition, a higher percentage (HIPAA wellness rules allow up to 50% of the total cost of coverage) would not be available for tobacco cessation programs that include any biometric screening or other medical testing. An employee who does not complete the health risk assessment or biometric screening cannot be denied access to a particular group health plan benefit package and the coverage provided to them under a benefit package cannot be limited.
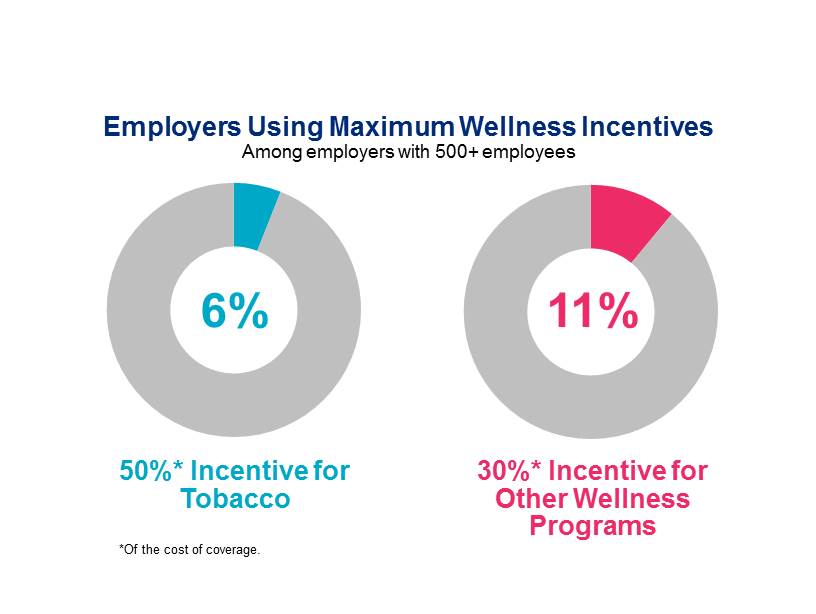
Despite the uncertainty that exists between the HIPAA and ADA rules, employers continued to add incentives in 2014 to encourage participation in health-related programs — or even to reward employees for meeting their health goals. But the practical implications of the EEOC proposal that limits incentives to 30% may be minimal. Most employers use incentives that are well below the maximum, and very few employers intend to increase incentives to the maximum.
ACA raised limits on wellness incentives: How will large employers respond? |
|
| Will use the maximum 50% incentive for tobacco | 6% |
| Will increase incentive for tobacco, but not to the maximum | 13% |
| Will use the maximum 30% for other wellness program(s) | 11% |
| Will increase the incentive for other wellness program(s), but not the maximum amount | 23% |
| Not considering adding or increasing incentives | 67% |
Source: Mercer
In addition, the most effective incentives for improving health and productivity lie beyond the realm of employee discounts or surcharges on health plan premiums. Research shows that financial incentives may help to increase awareness and drive short-term engagement, but when implemented alone, they fail to produce long-term, sustained changes in health risks. Some effective wellness programs don’t involve financial incentives at all.
Ultimately, the goal of any wellness program is to foster each individual’s intrinsic motivation to improve health. If employees feel that being healthy is part of “who we are” at the workplace, they are more likely to maintain long-term behavior change.
To learn more about the latest thinking on wellness, read Susan’s new article, “Going Beyond Wellness to Well-being,” published in the May 2015 issue of Workspan.
