Infusing Quality into your Network Strategy

A medical network evaluation can be one of the most impactful actions an employer can take to inform a successful healthcare benefits strategy. A view into care quality – however you choose to measure it – is key to understanding how a network drives value for plan members.
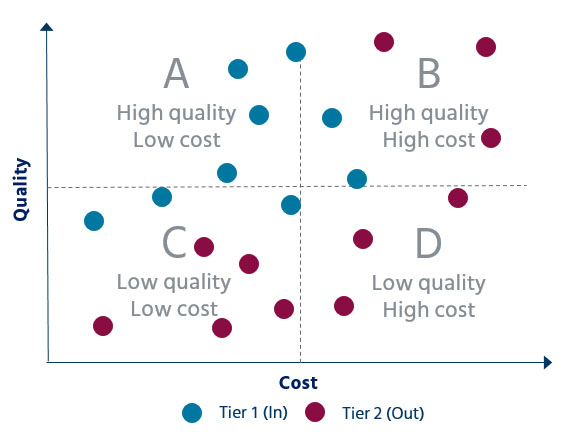
Mercer recently conducted a nationwide analysis of some of the major medical networks. We found that the largest value differentiator is around cost – in this case, discounts. Nationally, discounts among broad networks can differ by as much as 6%, while the quality and efficiency of the networks often differ by less than 1%. Alternative networks show a wider range of results, although variation by cost – as much as 10% compared to their broad network counterparts -- is still greater than variation in quality and efficiency.
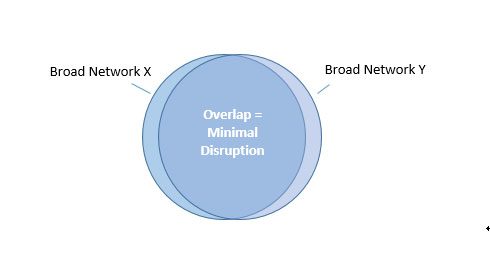
Broad network overlap makes differentiation harder to achieve
We weren’t shocked by these early results, since we know from years of performing disruption analysis for employers how much overlap exists between broad networks today. Without serious steerage efforts, the providers that an employer’s members see today would be more or less the same under a different broad network.
That isn’t to say that these different networks have the same value proposition. There are numerous features that could distinguish one from another, including fixed access fees, variable fees for out-of-network shared savings, as well as discounts. All of these, however, are ways to differentiate based on cost rather than overall quality. We do see more quality variation within different categories of care, so strategies that steer members to centers of excellence, for example, are still useful ways to get more value from a broad network arrangement.
Alternative networks offer another option
In the last few years there has been a proliferation of alternative network products coming to market. While these can take many forms, typically they are built by curating the broad network provider listing down to a smaller roster, often according to a proprietary algorithm that is supposed to incorporate elements of both quality and cost. Conceptually, it should look like this:
However, we have found that in some alternative networks, the distinction between providers in the broad and alternative network isn’t always that clear.
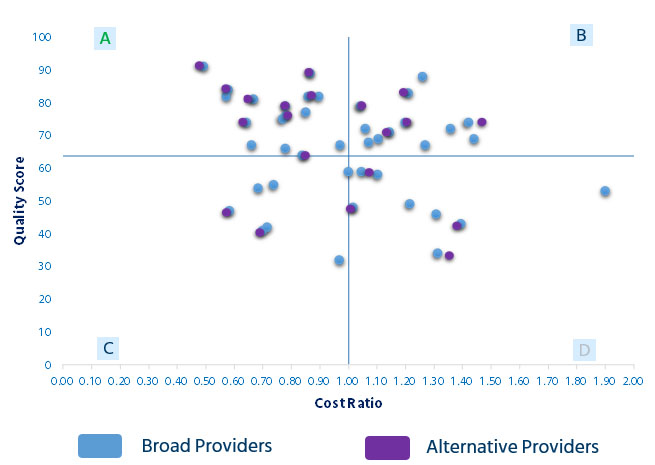
Mercer’s QualPic tool has been able to help our clients understand which alternative networks have significantly better quality, based on external data rather than statements made by carriers during a medical marketing exercise.
Moving to an alternative network will typically result in more provider disruption than moving from one broad network to another:
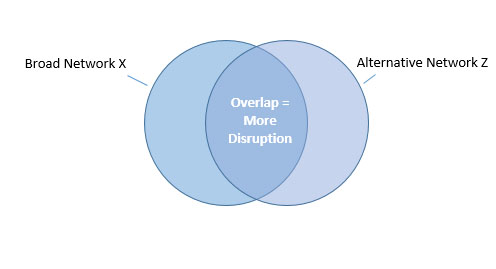
But accepting a certain level of disruption may be a necessary trade-off if quality is to become a true pillar in a network evaluation strategy. It will be easier to communicate the change to employees if you can feel confident that they and their family members will receive better care, and perhaps even pay less for it.
What’s next?
As we’ve seen when conducting network analyses with our Qualpic tool, the capability to infuse quality and efficiency into the evaluation process can be a game-changer for employer health plan sponsors looking to partner with the right carrier. The next time you’re considering a network change or any other solution that seeks to steer members to certain providers, make sure to include quality as part of your evaluation criteria.
