Opioid and Alcohol Abuse – Employers are Taking Action

For employers grappling with substance use disorders in the workforce, it can seem as if we’re in a “perfect storm” moment: the worsening opioid epidemic, a shortage of behavioral healthcare providers, and the continued stigma around substance use serves as a strong barrier to raising awareness, engaging in conversation and encouraging those at risk to seek help. Adding to the challenges is the cultural acceptance of alcohol use (and increasingly, other substances such as cannabis). In our recent 10-Minute Survey on Behavioral Health Care (results available here), about a fourth of survey respondents (and nearly a third of those with 5,000 or more employees) said that opioid use disorders pose a concern for their organization – and even more said alcohol use is a problem. The survey showed that some employers have found ways to navigate these challenges.
While there are a number of actions employers can take to address substance abuse in general and opioid use disorders in particular, about two-fifths of respondents – 41% – say they have yet to act. Overprescribing has been a major contributor to the opioid epidemic, and employers have begun to push their health plans and dental carriers to monitor the prescribing behavior of network providers. They also have begun to push pharmacy benefit managers to use evidence-based formularies restricting access to dangerous levels of pain meds. About a fourth of all survey respondents – but nearly half of those with 5,000 or more employees – say they have taken each of these steps.
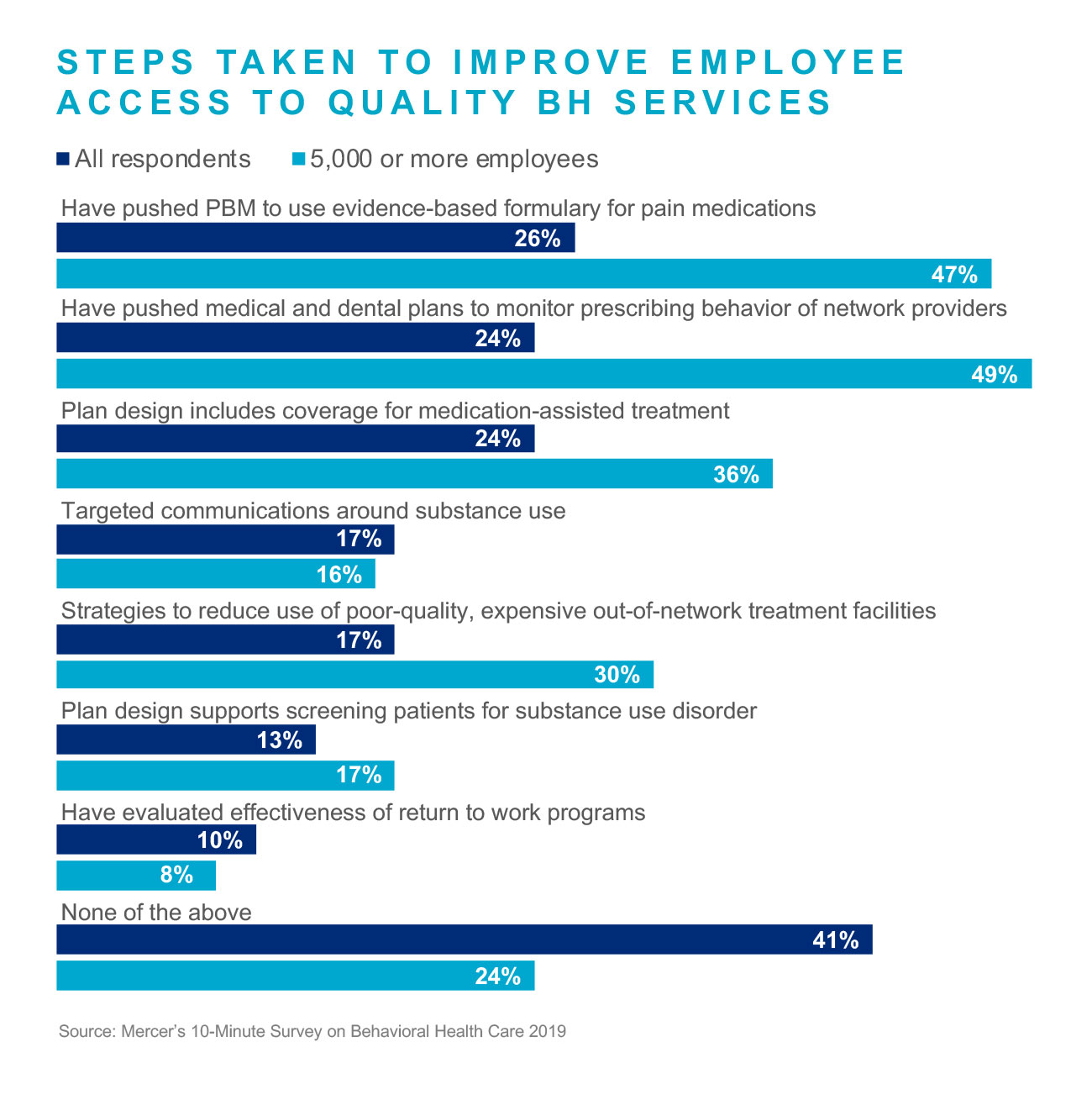
It is important that health care providers screen their patients for substance use and, if a problem is identified, that they can quickly get that individual the necessary services. For opioid use disorder, this includes having good access to medication-assisted treatment (MAT), which has been proven to stabilize people and allow them to successfully engage in ongoing treatment. About a fourth of respondents have ensured members have coverage for MAT.
One of the challenges that employers face is the proliferation of out-of-network treatment facilities that are very expensive and have poor track records for treatment success. Behavioral health and medical carriers have been working hard to identify high-quality, in-network treatment facilities, including Centers of Excellence. Promoting these facilities and steering individuals to them through advocacy programs and a well-integrated EAP can improve outcomes and the impact of the benefit dollar. Just 17% of all survey respondents – but 30% of those with 5,000 or more employees – have strategies to reduce the use of out-of-network treatment facilities.
Across our client base, we see increased prevalence of substance use disorders among adult dependents, ages 18 -24. Education about substance use, impairment and abuse, along with the myriad of assessment and treatment options offered by most employers is a good way to equip families with information they need to be aware – and find the right (in-network) resources should the need arise.
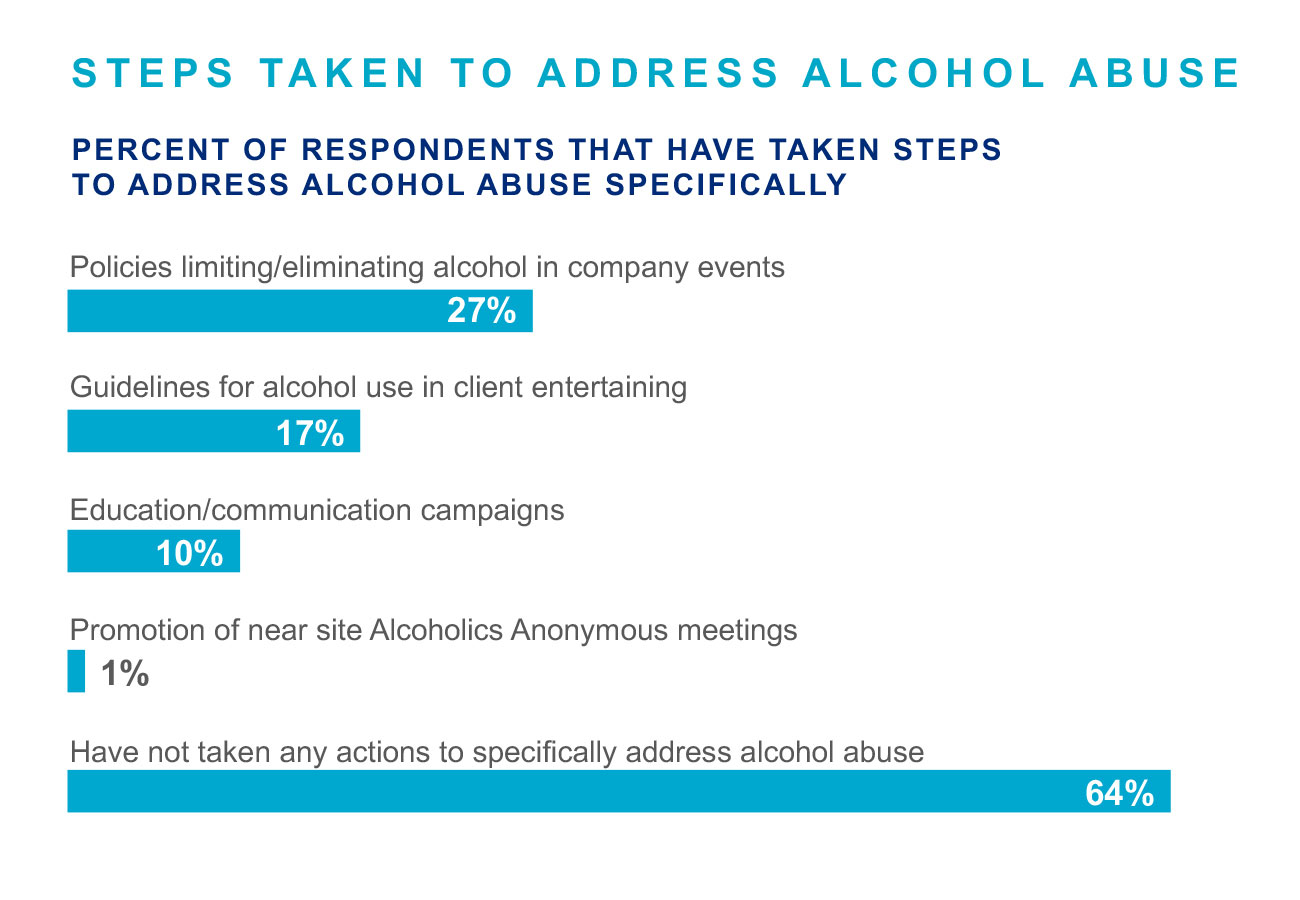
Regarding alcohol abuse in the workforce, nearly two-thirds of respondents (64%) have not taken steps to address this issue specifically. Just over a quarter of employers have policies limiting or eliminating alcohol at company events, and 17% have guidelines for alcohol use in client entertaining.
Our understanding of substance use disorder as a chronic condition has guided the development of more deliberate return to work programs and support for recovery services. This can take the form of an enhanced EAP offering, supervisor and manager training, and access to recovery-support programs that minimize the risk of relapse. Only one in 10 respondents have analyzed the effectiveness of their return to work programs; this is an important area of opportunity for employers – more individuals will require treatment, and potentially, time from work in their recovery journey. In the long run, this may be the most beneficial time spent by an employer given that workers in recovery – who report receiving substance use treatment in the past and who have not had a substance use disorder within the last twelve months – miss the fewest days from work of any group, including the general workforce.
For the full results of the 10-Minute Survey on Behavioral Health Care, download the full report here.
Authors:
Alisa Trugerman, Principal Total Health Management
Sandra Kuhn, Principal, Total Health Management
Beth Umland, Director of Research, Health & Benefits

